ISSN 2410-5708 / e-ISSN 2313-7215
Year 13 | No. 37 | June - September 2024
© Copyright (2024). National Autonomous University of Nicaragua, Managua.
This document is under a Creative Commons
Attribution-NonCommercial-NoDerivs 4.0 International licence.
Non-pharmacological diagnostic and therapeutic approach, obsessive-compulsive disorder in adults. Systematic review
https://doi.org/10.5377/rtu.v13i38.19123
Submitted on february 13th, 2023 / Accepted on august 28th, 2024
René Alfonso Aburto Gutiérrez
General Physician and Master in Epidemiology.
MINSA code 11169,
Doctoral student CIES UNAN- Managua.
Fernanda Pineda Gea
Prosthetic Audiologist and General Physician.
Master in Education, University Teaching and Research, USMP, Peru
Carlos Manuel, Téllez Ramos
MSc. in Higher Education in Health-UNAN, León
María Sol Pastorino
Ph.D. PhD in Social Sciences
Foreign teacher from the National Autonomous University of Nicaragua, Managua-CIES
Section: Health and social services
Scientific research article
Keywords: Obsessive-Compulsive Disorder, Cognitive-behavioral therapy, Adults
Abstract
To synthesize evidence of the non-pharmacological diagnostic and therapeutic approach in adults with obsessive compulsive disorder (OCD). Design: systematic review, including 9 case reports. Using MEDLINE, PUBMED, Google Scholar, Scielo, institutional repositories, thesauri: "Obsessive Compulsive Disorder AND Adult NOT Children". Inclusion criteria: Scientific articles published between 1990-2023, published in Spanish and English. Results: 9 included articles (nine patients) published in Spanish, eight published in Spain. The mean age was 29.6 years, and 68% of cases ranged from 20.8 to 38.4 years, with five patients in the second decade of life at the time of therapy and three in the third decade. The mean age of onset of symptoms is 21.12 years, and the onset of symptoms related to a stressful life event, female sex is the most affected. The Intrusive Thought Pattern prevailed. Psychotherapy combined with acceptance and commitment techniques was effective in eliminating psychological rigidity, with a frequency of once a week lasting between 45 to 60 minutes, and an average duration of 23.3 weeks, ranging from 8 weeks to 48 weeks, depending on the severity of your symptoms.
Conclusions: intrusive thoughts and female sex are prevalent aspects, affect the young population, psychological therapy is effective, patients present improvement of obsessive-compulsive symptoms even reaching subclinical levels, cognitive-behavioral therapy was the best directed by a therapist, with weekly sessions of one hour, face to face, from 8 to 43 weeks duration.
1. Introduction
Obsessive-Compulsive Disorder (OCD) is a mental health disorder that is characterized by the presence of recurrent obsessions and compulsions. Although pharmacological treatments, such as Selective Serotonin Reuptake Inhibitors (SSRIs), are effective in the management of OCD, non-pharmacological therapies are also used to complement or replace medication. Abramowitz et al. (2009) mention that one of the most common non-pharmacological therapies used in OCD is Cognitive Behavioral Therapy (CBT). CBT for OCD usually involves two main components: exposure therapy and response prevention. Exposure therapy involves gradually exposing the individual to the situations, thoughts, or images that trigger their obsessions. As the individual is repeatedly exposed to these feared stimuli, their anxiety gradually decreases. Response prevention involves resisting the compulsion that follows the obsession, which helps to interrupt the obsession-compulsion cycle. On the other hand, Abramowitz et al. (2009) describe that another non-pharmacological therapy used in OCD is acceptance and commitment therapy (ACT). ACT focuses on helping individuals accept their obsessive thoughts without trying to suppress or control them.
OCD affects 2-3% of the population. One-third of patients respond poorly to conventional therapies (McLaughlin et al., 2023). 90% of people with OCD also meet the diagnostic criteria for a co-occurring condition of depression, post-traumatic stress disorder, eating disorders, schizophrenia, hoarding disorder (Pinciotti, 2022) as well as suicidality, functional impairment, and days of home confinement (Weingarten et al., 2016).
Although OCD has a profound impact on the quality of life and daily activities of those who live with this disorder, it impacts the whole family. The time gap it takes to reach the diagnosis of OCD and then to the ideal therapy makes OCD a disorder that must be prioritized in public health, this research reviews the existing and accessible literature, addresses the diagnosis and non-pharmacological therapeutic behaviors used in the patient with OCD, emphasizing the two non-pharmacological therapies described in the previous paragraphs, makes a comparative analysis between the benefits of these therapies described and evidenced in the medical literature.
Posing the clinical (research) question in PECOS mode
What is the available evidence on the non-pharmacological diagnostic and therapeutic approach in adults with obsessive-compulsive disorder?
Population: Adults with OCD
Exposure: Non-pharmacological therapy, Type of non-pharmacological therapy for OCD: a. Cognitive-behavioral therapy, b. Acceptance and commitment therapy c. Exposure therapy and response prevention.
Control: No comparison was established
Outcome :
•Epidemiological profile of OCD; Age, Sex, Diagnostic age
•OCD symptom dimensions; Pattern of contamination. The pattern of pathological doubt. Intrusive thought pattern. Symmetry pattern.
•Clinical outcomes; Clinical Improvement, Duration of Therapy
STUDIES (Type of study): Observational studies (Clinical cases, case-control, analytical cross-sectional, cohorts)
2. Material and Methods
Type of Study: Systematic, prognostic, ambispective review with a qualitative approach
This review at the beginning of the study about the chronology or occurrence of the events and the recording of the information is ambispective because the units of analysis (articles, theses) record information that occurred in the past tense (retrospective) and according to the registration and search of the information making use of the tools (database, repositories, metasearch engines, etc.) it is prospective. It has a qualitative approach since the processing and analysis of the information was limited to recording and describing the relevant findings extracted from the units of analysis based on the PECOS variables established for this research, that said, no inferential statistical processing (meta-analysis) was performed.
Eligibility Criteria
Inclusion criteria:
•Type of publication: Scientific articles or gray literature with observational methodological design (report or series of cases, case-control, cross-sectional, cohort).
•Quality, methodology, or degree of evidence: to homogenize the level of evidence analyzed, it was decided to standardize the research design included in this study (See section, bias control).
•Accessibility: Scientific articles with Open Access, i.e. not only can the article or monographic thesis be read on the journal’s website or repository, but it can also be downloaded in pdf format.
•Language of publication: Scientific articles and monographic theses published in Spanish and/or English, as the latter represents up to 90% of the published evidence.
•Publication Period: Scientific articles published during 1990-2023 are available during the literature search period established in this review.
•Publication content: Studies addressing non-pharmacological therapies implemented in adult patients diagnosed with OCD.
Exclusion criteria:
•Clinical trial presentations, systematic reviews.
•Published studies in languages other than English or Spanish.
•Studies published outside the study period and search period.
• Studies with restricted access.
•Studies that do not address the subject in question.
Sources of information: Scientific articles and monographic theses are included in this review.
Information search technique (Articles and/or monographic theses)
Tools selected to search for information:
The search for the primary scientific articles was carried out using the following tools, such as metasearch engines and databases with free online access, the search for the monographic theses was carried out in Nicaraguan institutional repositories.
Database, Metasearch Engines, Repositories:
Database:
MEDLINE through the PUBMED search engine: https://pubmed.ncbi.nlm.nih.gov/, LILACS (Latin American and Caribbean Literature in Health Sciences) https://lilacs.bvsalud.org/es/,
Cochrane Controlled Trials Register (CENTRAL) y Cochrane Database of Systematic https://www.cochranelibrary.com/central/about-central,
BIREME.BR: https://bvsalud.org/es/
Metasearch engines:
Google Scholar: https://scholar.google.com.ni,
Repositories
CNU Repository, Nicaragua: https://repositorio.cnu.edu.ni/,
UNICA Repository, Nicaragua: https://repositorio.unica.edu.ni/
Bibliographic search strategy
The search strategy implemented in this review rigorously complies with the steps described by Pineda-Gea et al. (2023)
Step 1: Identification of search terms (thesauri): DeSC (Descriptors in Health Sciences).
The link to the health descriptors (https://decs.bvsalud.org/es/) page was accessed, while on the page we proceeded to type the search terms that were related to the PECOS variables expressed in clinical terms, to convert them into thesauri and later used in the search strategy previously designed to be applied in the database making use of the metasearch engines selected as search tools implemented in this research.
Step 2: Check for similarities of DeSC descriptors with MeSH descriptors
To corroborate if the DeSC descriptors are similar to the MeSH, we proceeded to read the concept of the descriptor, assuring us that it referred to the conceptual definition attributed to the clinical term adopted in this research, the previous procedure was carried out for each PECOS variable.
Table 1
Similarity of descriptors found in DeSC and MeSH
|
PECO variables expressed in clinical terms |
Descriptors DeSH |
Descriptor ID |
Descriptors Mesh |
||
|
P |
Adult |
Adult |
D000328 |
Adult |
|
|
Obsessive-Compulsive Disorder Compulsive Personality Disorder Compulsive Personality Obsessive-Compulsive Personality |
Obsessive-Compulsive Neurosis Anancastic Personality |
D009771 |
Obsessive-Compulsive Disorder |
||
|
D003193 |
Compulsive Personality Disorder |
||||
|
And |
Non-pharmacological treatment Acceptance and Commitment Therapy Virtual Reality Exposure Therapy |
Cognitive Psychotherapy Cognitive Psychotherapies Cognitive Therapy Cognitive Behavioral Therapy Cognitive Behavioral Therapy Cognitive Behavior Therapy Cognitive Behavioral Therapies Cognitive-Behavioral Therapies Cognitive Behavioral Therapies |
D015928 |
Cognitive Behavioral Therapy |
|
|
D064869 |
Acceptance and Commitment Therapy |
||||
|
D063367 |
Virtual Reality Exposure Therapy |
||||
|
C |
No comparison variable was established |
||||
|
Or |
Epidemiological profile |
Age |
Age Group Age Group Age Groups Age Groups |
D009273 |
Age Groups |
|
Age and Sex Distribution |
DDCS050271 |
Age and Sex Distribution |
|||
|
Age Home |
Age of Disease Establishment |
D017668 |
Age of Onset |
||
|
Sex |
Sex |
D012723 |
Sex |
||
|
OCD Symptom Dimensions |
Contamination pattern |
Signs and Symptoms Clinical Manifestations Clinical Observations Clinical Observation Complaints and Symptoms Clinical Signs Clinical Symptom Symptoms |
D012816 |
Signs and Symptoms |
|
|
The pattern of pathological doubt |
|||||
|
Intrusive thought pattern |
|||||
|
Symmetry Pattern |
|||||
|
Clinical results |
Treatment Outcome Clinical Effectiveness Treatment Effectiveness Clinical Efficacy Treatment Effectiveness Patient-Relevant Outcome Rehabilitation Outcome |
D016896 |
Treatment Outcome |
||
|
S |
Studies |
Observational studies (clinical cases, case-control, analytical cross-sectional, cohorts) |
D064888 |
Observational Study |
|
Step 3: Build and define a search string
To make the bibliographic search within the databases and repositories more sensitive and specific, the use of Boolean operators were used as a strategy to be able to unify the search terms and define search phrases within the selected databases and repositories to expand the search strategy and at the same time make it more sensitive and specific to locate the scientific evidence that answers the question clinical analysis in this review.
Table 2
Example of search string execution and the results obtained in some of the selected tools for information search
Step 4: Apply search strategies:
For this systematic review, the descriptors MeSH and DeSC were used, whose similarity was corroborated by the unique identifier number. Within the databases, repositories, and metasearch engines used in this review, the steps described below should be followed:
1.The thesauri were typed independently for each MeSH or DeSH terms identified in steps one and two of the search strategy.
2.The combinations were made between them, making use of the Boolean operators described in step three and recorded in table two
3.Once the search term combined or not in the search engine of the tools used (databases, meta-search engines, and repositories) was typed, the filters or limits of the search strategy were executed, which were:
•Year of publication 1990-2023
• Publication language: English-Spanish
•Article type: Observational studies, systematic reviews, clinical trials, Age: Adults, No gender restriction,
•Full text available.
Bibliographic search period: Study period: last 33 years (1990- 2023)
Bibliographic search date: Start: June 1, 2023, End: July 30, 2023
Prism Diagram Process of searching, selecting, and including scientific articles
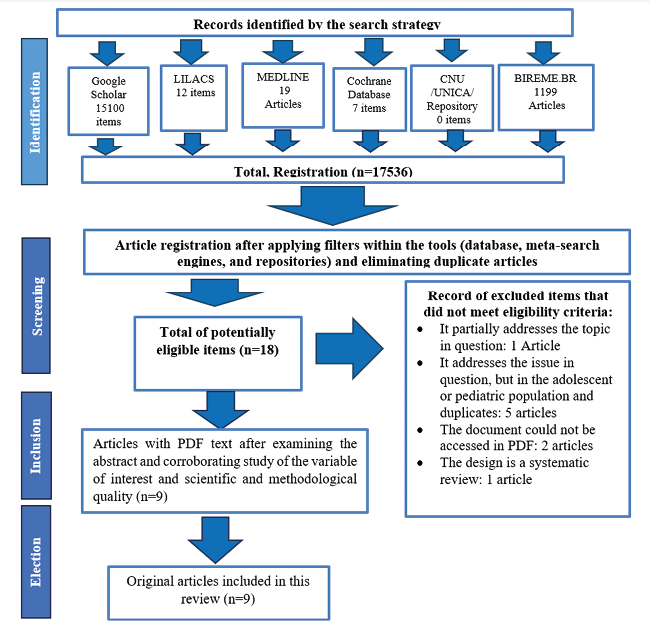
Source: Adapted from Pineda et al. (2023) Methodological aspects to be evaluated in a systematic review and PRISMA (2020).
Data Extraction Process: Data Analysis
The most relevant characteristics of the studies were unified using the finding summary table, which will reflect the data regarding the publication of the article (table 1) and the other aspects of the content (table 2), as well as the summary table of excluded articles (table 3), presented below:
Summary of findings: Publication date
|
N° Art. |
Author(s) / year of publication |
Post Type |
Country conducting research |
Publication language |
Research Title |
Journal in which it was published |
|
1 |
Behobi et al. (2013) |
Scientific Article |
Buenos aires- Argentina |
Spanish -English |
Individual Cognitive Psychotherapy of OCD |
Salud Ment vol.36 no.4 Mexico Jul./Aug. 2013 |
|
2 |
Carrió (2004) |
Scientific Article |
Valencia - Spain |
Spanish -English |
Long-Term Effects of Cognitive Treatment in a Case of Obsessive-Compulsive Disorder |
Journal of Psychopathology and Clinical Psychology, 9(2), 99–121. |
|
3 |
Ceballos and Orozco (2015) |
Scientific Article |
Madrid-Spain |
Spanish -English |
Application of cognitive-behavioral therapy in a case of obsessive-compulsive disorder |
Journal of Clinical Cases in Mental Health (2015) 1:79-100 |
|
4 |
Montero et al. (2013) |
Scientific Article |
Salamanca- Spain |
Spanish -English |
Cognitive-behavioral therapy with components of acceptance and commitment in a case of obsessive-compulsive disorder |
Journal of the Spanish Association of Neuropsychiatry, 33 (117), 123-134. |
|
5 |
Carcedo and Vindel (2008) |
Scientific Article |
Madrid- Spain |
Spanish |
Treatment of Obsessive-Compulsive Disorder from New Cognitive Perspectives: A Case Study |
Anxiety and Stress, 14, 321-339 |
|
6 |
De la Torre and Aguay (2017) |
Scientific Article |
Spain |
Spanish – English |
Acceptance and Commitment Therapy as the Treatment of Choice for OCD: A Case Study |
Journal of Psychotherapy, 28(106), 181-196 |
|
7 |
Manera (2015) |
Scientific Article |
Spain |
Spanish |
Exposure and Response Prevention in the Case of a Young Woman with Obsessive-Compulsive Disorder |
Journal of Clinical Psychology with Children and Adolescents, 2(1), 75-81. |
|
8 |
Martínez (2016) |
Grey Literature (Master’s Thesis) |
Elche-Spain |
Spanish |
Cognitive-behavioral treatment of a case of obsessive-compulsive disorder |
Institutional Repository |
|
9 |
Gil et al. (2001) |
Article |
Murcia -Spain |
Spanish |
Personality disorders and response to psychological treatment in a case of severe obsessive-compulsive disorder. |
Behavioral Psychology, 9(3), 609-627. https://www.behavioralpsycho.com/wp-content/uploads/2020/04/11.Moreno_9-3oa.pdf |
Table 2
Content of publications extracted based on the PECOS variables established in this research
|
N° Art. |
Research Design |
Period/sample |
Main Variables studied |
Main results |
Conclusions of the study |
Degree of evidence |
|
1 |
Case Presentation |
1 patient
|
Sociodemographic Characteristics •Age •Sex •Onset of symptoms Dimensions of OCD Clinical results: •Type of Therapy •Duration of therapy •Improvement of symptoms |
Sociodemographic characteristics: Age: 49 years old Symptom onset: 20 years Gender: Male Dimensions of OCD: Intrusive Thoughts Pattern, Symmetry Pattern, Pathological Doubt Pattern, Contamination Pattern. Obsessions with pollution and dirt, patient, avoidant behavior Obsessions of doubt about obsessive doubts about certain types of issues related to home security. Computer rituals: The patient developed an overlap between Internet addiction and OCD, since the patient had to play in a stereotypical and ritualistic way, winning in a certain order and having to restart the game at the slightest mistake. Clinical results: Type of therapy: Individual cognitive psychotherapy Duration: one hour a week for 20 weeks. Improvement of symptoms: The patient was evaluated with scales: Yale-Brown Obsessions and Compulsions Scale (YBOCS), Clark-Beck Obsessive-Compulsive Inventory (C-BOCI), and Revised Obsessive Beliefs Inventory (ICO-R) moving from a classification of OCD symptom intensity from Very Severe to Moderate |
The intervention was limited to specific factors cognitive change, attention to non-specific factors as empathy, acceptance, and commitment to change, were of primary importance in the treatment of the patient |
Observational study Level of evidence Mild |
|
2 |
Case Presentation |
1 patient
|
Sociodemographic Characteristics •Age •Sex •Onset of symptoms Dimensions of OCD Clinical results: •Type of Therapy •Duration of therapy •Improvement of symptoms |
Sociodemographic characteristics: Age: 31 years old Onset of symptoms: 30 years Gender: Female Dimensions of OCD: Intrusive thought pattern: Self-harm, the need to compulsively check the gas key and the lock on the door of your house Clinical results: Type of therapy: Individual cognitive psychotherapy Duration: one hour a week for 22 weeks. Improvement of symptoms The patient was evaluated with the Yale-Brown Obsessions and Compulsions Scale (YBOCS), the Clark-Beck Obsessive-Compulsive Inventory (C-BOCI), and the Revised Obsessive Beliefs Inventory (ICO-R), moving from a classification of OCD symptom intensity from Moderate to a score below the subclinical level (0 points) one year after the end of treatment. |
The assessment with the scales used in this research was effective since the scores in it decreased clearly and progressively until they disappeared one year after the end of the treatment, the pharmacological management acted as an adjuvant to the psychological treatment by improving the patient’s mood |
Observational study Level of evidence Mild |
|
3 |
Case Presentation |
1 patient
|
Sociodemographic Characteristics •Age •Sex •Onset of symptoms Dimensions of OCD Clinical results: •Type of Therapy •Duration of therapy •Improvement of symptoms |
Sociodemographic characteristics: Age: 25 years old Symptom onset: 12 years Gender: Female Dimensions of OCD: Intrusive Thought Pattern, Pathological Doubt Pattern Poor symptom recognition, moderate avoidance, moderate indecision, severe excessive sense of responsibility, mild slowness, moderate pathological self-doubt, and moderate global severity with moderate interference with daily life Clinical results: Type of therapy: Individual cognitive psychotherapy Making use of the following techniques: Psychoeducation, Cognitive Restructuring, Diaphragmatic Breathing, Autogenic Training, Exposure, Self-Instructions and Self-Recordings Duration: one hour a week for 25 weeks. Improvement of symptoms The patient was evaluated with the Yale-Brown Obsessions and Compulsions Scale (YBOCS), Clark-Beck Obsessive-Compulsive Inventory (C-BOCI), and Revised Obsessive Beliefs Inventory (ICO-R) scales, an improvement of up to 60% of symptomatology was observed one year after the end of treatment |
Although the symptoms have been reduced from considerably, increasing the patient’s quality of life has not been achieved Psychotherapy is effective in patients with OCD, however, this effectiveness has been closely related to the patient’s collaboration with OCD. Time to perform out-of-office tasks |
Observational study Level of evidence Mild |
|
4 |
Case Presentation |
1 patient |
Sociodemographic Characteristics •Age •Sex •Onset of symptoms Dimensions of OCD Clinical results: •Type of Therapy •Duration of therapy •Improvement of symptoms |
Sociodemographic characteristics: Age: 33 years old Onset of symptoms:31 years Gender: Female Dimensions of OCD: Pattern of intrusive thoughts and obsessions Pattern of contamination Avoidance and Self-imposed restrictions, verification, repeated cleaning, repeated reassurance-seeking Clinical results: Type of therapy: Cognitive-behavioral therapy (CBT) and Acceptance and Commitment (ACT) + Serotonin reuptake inhibitors Duration: 45 minutes once a week for 8 weeks. Improvement of symptoms It does not detail the scales used for the patient’s evolution. There was a progressive decrease in the number of rituals and in the anxiety they generated, until their total disappearance at the end of the treatment. |
The addition of ACT techniques to CBT+SSRIs produces the greatest benefits in the treatment of OCD, which translate into a greater remission of symptoms, a generalization to other areas of the life of the person and the maintenance of improvement. |
Observational study Level of evidence Mild |
|
5 |
Case Presentation |
1 patient
|
Sociodemographic Characteristics •Age •Sex •Onset of symptoms Dimensions of OCD Clinical results: •Type of Therapy •Duration of therapy •Improvement of symptoms |
Sociodemographic characteristics: Age: 27 years old Symptom onset: 27 years Gender: Male Dimensions of OCD: Intrusive Thought Pattern, Pathological Doubt Pattern Obsessions of doubt: They are obsessed with the possibility of making mistakes when dispensing prescriptions, making a catastrophic assessment of responsibility. Verification rituals: The patient checks again and again if any errors have occurred Clinical results: Type of therapy: Individual cognitive psychotherapy + Serotonin receptor inhibitors Duration: one hour a week for 32 weeks. Improvement of symptoms: The patient was evaluated with the Yale-Brown Obsessions and Compulsions Scale (YBOCS), the Clark-Beck Obsessive-Compulsive Inventory (C-BOCI), and the Revised Obsessive Beliefs Inventory (ICO-R), moving from a classification of the intensity of OCD symptoms to an improvement and reduction of symptoms, during follow-up, there were no relapses, therefore the therapy was effective in this patient. |
It is considered that the emphasis on cognitive techniques as the basis of exposure has not only reduced the symptomatology but that the changes have been maintained in the follow-up and even in some cases have improved, reinforcing the hypothesis that maintains that the use of cognitive techniques could have a prophylactic effect in the prevention of relapses. |
Observational study Level of evidence Mild |
|
6 |
Case Presentation |
1 patient |
Sociodemographic Characteristics •Age •Sex •Onset of symptoms Dimensions of OCD Clinical results: •Type of Therapy •Duration of therapy •Improvement of symptoms |
Sociodemographic characteristics: Age: 23 years old Symptom onset: 14 years Gender: Male Dimensions of OCD: Contamination Pattern, Symmetry Pattern Symmetry obsessions with compulsions to tidy up, fix, and repeat Contamination obsessions with washing and cleaning compulsions Clinical results: Type of therapy: Commitment acceptance therapy Duration: one hour once a week for 18 weeks. Improvement of symptoms A progressive decrease in symptoms was recorded from the first session they generated, until their total disappearance at the time of completion of treatment |
Acceptance and commitment therapy can be a useful, effective approach without psychosomatic adverse effects, implementable both in health care contexts and in private practice, for the treatment of severe obsessive-compulsive disorder, since it makes it possible to reduce the symptoms of the disorder, maintains therapeutic adherence and acts to improve the quality of life of the person |
Observational study Level of evidence Mild |
|
7 |
Case Presentation |
1 patient |
Sociodemographic •Age •Sex •Onset of symptoms Dimensions of OCD Clinical results: •Type of Therapy •Duration of therapy •Improvement of symptoms |
Sociodemographic characteristics: Age: 18 years old Symptom onset:18 years Gender: Female Dimensions of OCD: Intrusive thought pattern rituals of verification that appear in your house (apartment or villa) and verify that the doors of your house are not open and close them He checks several times if he has everything he needs in his bag (mobile, purse, keys, etc.), he also does it when he keeps it in the locker of his work and school Clinical results: Type of therapy: exposure and response prevention (ERP) treatment along with pharmacological treatment Duration: one hour once a week for 15 weeks. Improvement of symptoms There was a decrease in the rate of anxiety and the number of compulsions and obsessions carried out |
A progressive and significant reduction in avoidance behaviors and compulsions related to verification has been achieved, observing that exposure treatment and response prevention are effective in reducing symptoms, with the patient being the protagonist of this therapy |
Observational study Level of evidence Mild |
|
8 |
Case Presentation |
1 patient |
Sociodemographic Characteristics •Age •Sex •Onset of symptoms Dimensions of OCD Clinical results: •Type of Therapy •Duration of therapy •Improvement of symptoms |
Sociodemographic characteristics: Age: 27 Onset of symptoms: Not described Gender: Female Dimensions of OCD: Symmetry Pattern Compulsions Checking and Order Clinical results: Type of therapy: cognitive-behavioral combined exposure with response prevention and cognitive restructuring, in addition to training in abdominal breathing and pharmacotherapy. Duration: one hour a week for 22 weeks. Improvement of symptoms The patient was evaluated with the Yale-Brown Obsessions and Compulsions Scale (YBOCS), the Clark-Beck Obsessive-Compulsive Inventory (C-BOCI), and the Revised Obsessive Beliefs Inventory (ICO-R). At the end of the intervention, the obsessions and compulsions, and there was an improvement in both anxiety levels and depressive symptomatology. A first follow-up interview was conducted one month later, in which the patient’s clinical improvement was maintained. of the symptoms one year after the end of the treatment |
Cognitive-behavioral therapy that combines exposure with response prevention and cognitive restructuring, as well as abdominal breathing training and pharmacotherapy, is effective in the treatment of OCD |
Observational study Level of evidence Mild |
|
9 |
Case Presentation |
1 patient
|
Sociodemographic Characteristics •Age •Sex •Onset of symptoms Dimensions of OCD Clinical results: •Type of Therapy •Duration of therapy •Improvement of symptoms |
Sociodemographic characteristics: Age: 33 years old Symptom onset: 17 years Gender: Male Dimensions of OCD: The pattern of pathological doubt, the pattern of intrusive thoughts Patient suffers from Severe OCD: Self-harm, and continuous doubt about “the true intentions” of their therapist. The obsessive fear of not paying. Clinical results: Type of therapy: Cognitive-behavioral psychotherapy Duration: one hour a week for 4 years. Improvement of symptoms The patient was evaluated with the Yale-Brown Obsessions and Compulsions Scale (YBOCS), Clark-Beck Obsessive-Compulsive Inventory (C-BOCI), and Revised Obsessive Beliefs Inventory (ICO-R) Improvement in OCD symptomatology was observed |
The cognitive-behavioral model offers sufficient sssscientific and clinical guarantees for OCD, however, it presupposes the patient collaboration is an extreme that is not always verified in the clinic. |
Observational study Level of evidence Mild |
Table 3
Potentially eligible items that were excluded during the screening phase
|
Excluded item characteristics |
||||
|
N° Art |
Author(s) / Year |
Título de la investigation |
Criteria you don’t meet |
Published |
|
Ramos-Cejudo and Cano-Vindel (2008) |
Cognitive-behavioral treatment of a case of generalized anxiety disorder: The metacognitive component |
It partially addresses the issue in question |
Anxiety and Stress Journal 14(2-3), 321-339. |
|
|
2 |
Fernández-Montes and García (2019) |
Cognitive-behavioral treatment in an adolescent with obsessive-compulsive disorder |
It addresses the issue in question but in the adolescent population Duplicate |
Journal of Clinical Cases in Mental Health, 7(1), 39-61. https://ojs.casosclinicosensaludmental.es/index.php/RCCSM/article/view/43 |
|
3 |
Ulloa et al. (2011) |
Ulloa FRE, Palacios CL, Sauer VTR. Obsessive-Compulsive Disorder in Children and Adolescents: A Review of Treatment. |
It addresses the issue in question but in the adolescent and pediatric population |
Salud Mental. 2011; 34 (5):415-420. |
|
4 |
Barboza et al. (2023). |
Intervention from the cognitive behavioral model for the treatment of OCD (Obsessive Compulsive Disorder) in young adults. |
The full PDF document could not be accessed |
Simón Bolívar University repository available: https://bonga.unisimon.edu.co/handle/20.500.12442/12294 |
|
5 |
Field (2023) |
Efficacy of Internet-Based Cognitive Behavioral Therapy for Obsessive-Compulsive Disorder: A Systematic Review. |
The document cannot be accessed directly, the design is a systematic review |
Repository European University of the Atlantic. Available: https://repositorio.uneatlantico.es/id/eprint/6236/ |
|
6 |
Rosa-Alcázar et al. (2012) |
Efficacy of cognitive-behavioral treatments in obsessive-compulsive disorder in children and adolescents: a qualitative review. |
It addresses the issue in question but in the adolescent and pediatric population Duplicate |
Annals of Psychology, 28 (2),313-326. ISSN: 0212-9728. https://www.redalyc.org/articulo.oa?id=16723135002 |
|
7 |
Petrizán et al. (2017) |
The cognitive approach in the treatment of an adolescent with sexual obsessions and compulsions. |
It addresses the issue in question but in the adolescent population Duplicate |
Journal of Clinical Psychology with Children and Adolescents, 4(2),143-148. ISSN:. https://www.redalyc.org/articulo.oa?id=477152556007 |
|
8 |
Gutiérrez, and Rivero. (2019). |
Cognitive-behavioral therapy in the treatment of an adolescent with obsessive-compulsive disorder. |
It addresses the issue in question but in the adolescent population Duplicate |
Electronic Journal of Psychology Iztacala, 22(4). https://www.revistas.unam.mx/index.php/repi/article/view/72362 |
|
9 |
Falcón, Lazar and García (2012). |
The role of parents in the cognitive-behavioral treatment of obsessive-compulsive disorder in childhood: a case report. |
It addresses the issue in question but in the pediatric population |
Cuadernos de medicina psicosomática y psiquiatría de enlace, (102), 8. |
Study bias control
As can be seen in Table number three and the PRISMA diagram, those studies that did not meet the eligibility criteria, which are potentially eligible in the screening phase, were excluded. In the selection phase, the abstracts and titles of the potentially eligible monographic articles/theses were read three times after the critical reading. The STROBE tool (2009) was applied to assess the methodological quality of the articles, more than 90% of the evidence published under this line and research theme belonged to the case report design.
3. Results and Discussion of Results
A total of 18 articles were potentially identified after searching MEDLINE, LILACS, SCIELO, repositories, and metasearch engines, applying the respective filters and eligibility criteria to make the search more sensitive and specific, in the screening phase nine articles were excluded (summary table of findings three) leaving nine potentially eligible articles which, after being subjected to a critical reading of the abstract and content, I choose to include them in their entirety in this review, it is worth mentioning that the nine articles included in this review had a slight level of evidence because their design was case reporting. All were published in Spanish, 89% (8) of the articles were published in Spain, and 11% in Buenos Aires (1). This suggests that the clinical-epidemiological characterization of this clinical entity in the routine practice of Spanish health professionals is frequent and that priority is being given to publication so that we can all evidence this problem to intervene in it.
Sociodemographic characteristics recorded in the nine patients
Figure 1
Age Distribution of OCD Patients at the Time of Therapy and Symptom Onset
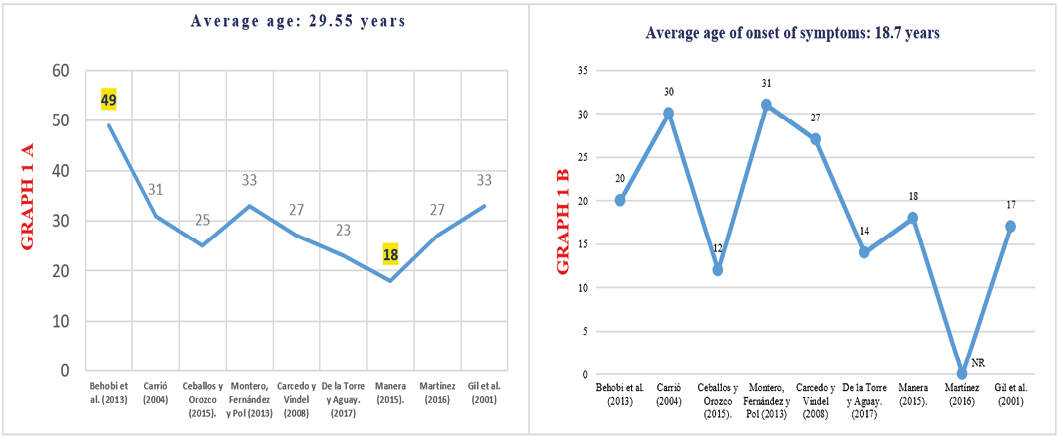
Source: Scientific evidence described in the summary table of findings two.
The average age of the patients studied was 29.5 years, +/- 8.7 years, the minimum age was 18 years (Manera 2015) and the maximum age was 49 years, reported by Behobi et al. (2013), with a mode of 33 years described in a study carried out by Montero, Fernández and Pol (2013) and Gil et al. (2001), the average age of symptom onset was 18.7 years. +/- 9.8 years, the youngest patient with the onset of symptoms was at the age of 12 years (Ceballos & Orozco, 2015) and the highest age for the onset of symptoms was 31 years, 44.4% of the patients studied were in the second decade of life, the nine patients diagnosed with OCD at the time of the consultation agreed that their symptoms were related to a critical incident that marked their behavior, the median age from the onset of symptoms and the beginning of therapy was 5.5 years, +/- 8.2 years, what we observed is that OCD affects people from a very early age affecting their integral development in social, family, education, work life and very likely in sentimental relationships.
55.5% of the patients studied belonged to the female sex, described by Carrió (2004), Ceballos and Orozco (2015), Montero, Fernández and Pol (2013), Manera (2015), Martínez (2016), although it was shown a higher percentage in women it is known that OCD affects both sexes equally, as described by Brock and Hany (2022) who showed that the incidence of OCD is practically similar, with a slight trend in favor of women.
Figure 2
Dimensions of OCD in the Included Patients
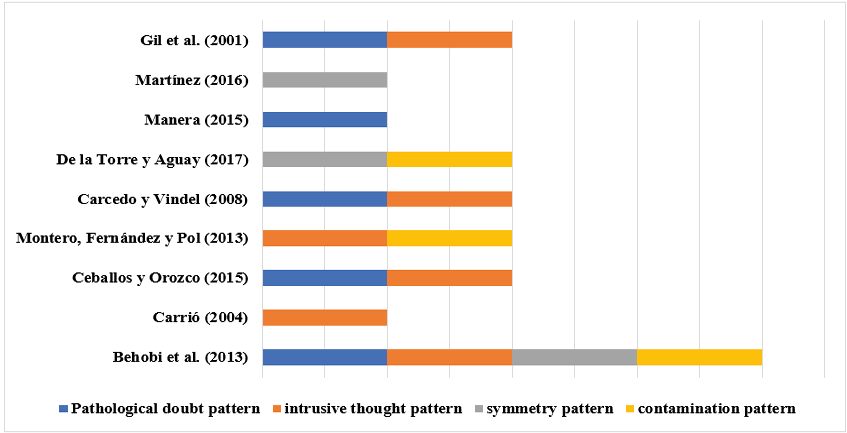
Source: Scientific evidence described in the summary table of findings two.
Regarding the predominant symptomatology, it was observed that the pattern of intrusive thoughts was described in six of the nine patients (66.6%) in research carried out by Gil et al. (2001), Behobi et al. (2013), Carrió (2004), Ceballos and Orozco (2015), Montero, Fernández and Pol (2013), Carcedo and Vindel (2008). It should be noted that the appearance of intrusive thoughts of a more or less unpleasant nature is common in most of the population, but what differentiates OCD is that they are egodystonic and bizarre and cause great emotional suffering to patients. By a chemical defect in the brain, the patient magnifies the value placed on thoughts (e.g., “I will be responsible for possible harm if I don’t check the gas”, “I am a horrible person thinking this”, “since I think this, I just wish it to happen; I am disgusting”, “if I do not control these thoughts, I will go crazy and be hospitalized”), then an irrational threat caused by that intrusive thought is perceived, discomfort/anxiety is produced and it is what gives rise to mental or physical compulsions as well as avoidances or mental ruminations as a way to find a little peace and all this ends up affecting the quality of life of patients.
Figure 3
Psychotherapy of OCD in the Included Patients
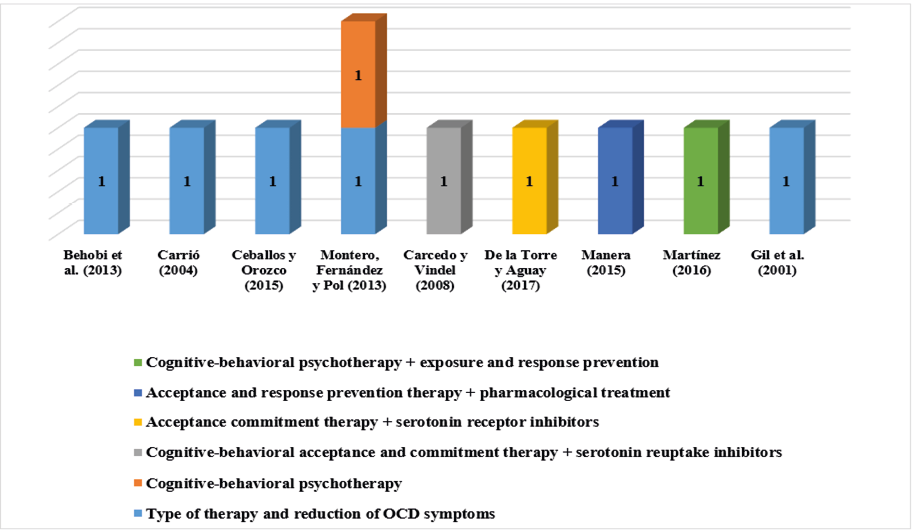
Source: Scientific evidence described in the summary table of findings two.
Type of therapy and reduction of OCD symptoms
The evidence consulted suggests that the objective of Psychotherapy combined with the different techniques of acceptance and commitment, is to eliminate psychological rigidity for which it employs some basic procedures such as acceptance, being in the present, the development and commitment to one’s values, the discovery of the self as a context and the deactivation of thought (cognitive defusion)). These procedures are related, in such a way that, if thought deactivation is applied, thoughts, feelings, emotions, and sensations are present and accepted, discovering and living the self as a context, the evidence included registers a reduction in some of the symptoms derived from associated disorders such as depression and anxiety and that increase or enhance the effects of OCD makes it possible for it to be reduced in a general way the intrusions and ruminations caused by the disease.
Figure 4
Duration of OCD Psychotherapy in Included Patients
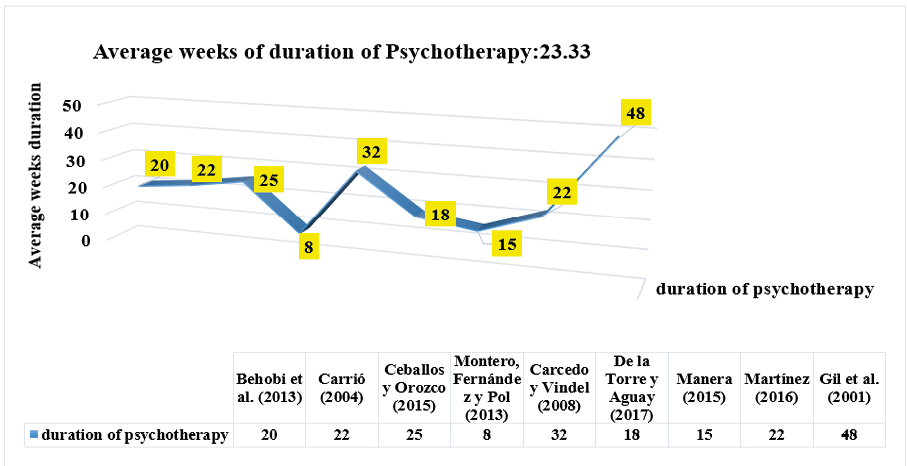
Source: Scientific evidence described in the summary table of findings two.
The frequency of psychotherapies described by the authors in the nine articles reviewed was once a week with a duration between 45 and 60 minutes per section. The duration of psychotherapy was variable among patients. The average duration of therapies was estimated to be 23.3 weeks, it was observed that the minimum duration of psychotherapy described in the consulted literature was 8 weeks recorded in a study carried out by Montero et al. (2013) and the maximum duration was 48 weeks described by Gil et al. (2001) whose patient had a diagnosis of severe OCD in which an evident improvement of clinical symptoms was observed after completion treatment. The findings suggest that the variability of the duration of psychotherapy in the patient with OCD will depend on the severity of their symptoms and the different measures of improvement used according to the included studies have been based on the pre-and post-therapy score obtained after the application of clinical instruments such as the Yale-Brown Obsessions and Compulsions Scale (YBOCS). Clark-Beck Obsessive-Compulsive Inventory (C-BOCI) and Revised Obsessive Beliefs Inventory (ICO-R).
Conclusiones
Obsessive-compulsive disorder begins at very early ages such as adolescence affecting personal and family development, there is no predilection for sex in this study the female sex was the most affected, many patients recognize the onset of this neuropsychiatric disease after a stressful life event, Obsessive Compulsive Disorder has a variety of clinical presentation ranging from mild to severe and disabling, The clinical dimensions are very varied, overlapping with each other, with intrusive thoughts being the most prevalent in this review, psychotherapies are effective, patients present significant improvement of obsessive and compulsive symptoms even up to subclinical levels of the disease during and after psychotherapy, the “gold standard” being cognitive-behavioral therapy directed by a therapist, with weekly one-hour, face-to-face sessions, from 8 to 43 weeks in length.
DECLARATION OF INTERESTS
Conflict of interest: The authors have declared no conflict of interest.
Funding source: none.
Ethical approval: Ethical approval was not required as this is a secondary analysis of data derived from published primary studies.
AUTHOR CONTRIBUTION
René Alfonso GUTIERRÉZ-ABURTO: Development of research protocol and report, data extraction, searches, study identification, analysis, and information processing.
Fernanda PINEDA-GEA: Review of protocol and research report, Assessment of the quality of data extraction, searches and identification of studies, data extraction, and preparation of first and last version of the manuscript for review.
Carlos Manuel TÉLLEZ RAMOS: Revision and correction of style, coherence of the content with the statement of the problem, objectives, analysis of the data, conclusions, and recommendations obtained.
María Sol PASTORINO: Content review, preparation of the latest version of the manuscript.
All authors have reviewed and approved the final version of the text.
References
Abramowitz, J.S., Taylor, S., & McKay, D. (2009). Obsessive-compulsive disorder. The Lancet, 374 (9688), 491–499. https://doi:10.1016/s0140-6736(09)60240-3
Brock, H., & Hany, M. (2022). Obsessive-Compulsive Disorder. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK553162/#article-26069.s9
Baer L. (1994). Factor analysis of symptom subtypes of obsessive-compulsive disorder and their relation to personality and tic disorders. The Journal of Clinical Psychiatry, 55 Suppl, 18–23. https://pubmed.ncbi.nlm.nih.gov/8077163/
Bloch, M. H., Landeros-Weisenberger, A., Rosario, M. C., Pittenger, C., & Leckman, J. F. (2008). Meta-analysis of the symptom structure of obsessive-compulsive disorder. The American journal of psychiatry, 165(12), 1532–1542. https://doi.org/10.1176/appi.ajp.2008.08020320
Behobi Baudou, Walter A., García, Fernando, & Fernández-Álvarez, Héctor. (2013). Individual cognitive psychotherapy of OCD. Mental Health, 36(4), 347-354. http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0185-33252013000400010&lng=es&tlng=es.
Carrió Rodríguez, C. (2004). Long-term effects of cognitive treatment in a case of obsessive-compulsive disorder. Journal of Psychopathology and Clinical Psychology, 9(2), 99–121. https://doi.org/10.5944/rppc.vol.9.num.2.2004.3972
Drubach D. A. (2015). Obsessive-compulsive disorder. Continuum (Minneapolis, Minn.), 21(3 Behavioral Neurology and Neuropsychiatry), 783–788. https://doi.org/10.1212/01.CON.0000466666.12779.07
Fals-Stewart, W., & Lucente, S. (1994). Behavioral group therapy with obsessive-compulsives: an overview. International journal of group psychotherapy, 44(1), 35–51. https://doi.org/10.1080/00207284.1994.11490733
Fernández-Montes Rodríguez, I., & García Sánchez, S. (2019). COGNITIVE-BEHAVIORAL TREATMENT IN AN ADOLESCENT WITH OBSESSIVE-COMPULSIVE DISORDER. Journal of Clinical Cases in Mental Health, 7(1). https://ojs.casosclinicosensaludmental.es/index.php/RCCSM/article/view/43
Leckman, J. F., Grice, D. E., Boardman, J., Zhang, H., Vitale, A., Bondi, C., Alsobrook, J., Peterson, B. S., Cohen, D. J., Rasmussen, S. A., Goodman, W. K., McDougle, C. J., & Pauls, D. L. (1997). Symptoms of obsessive-compulsive disorder. The American journal of psychiatry, 154(7), 911–917. https://doi.org/10.1176/ajp.154.7.911
Pineda Gea, F., Téllez Ramos, C. M.., & Gutiérrez Aburto, R. A... (2023). Methodology Applied in the Writing of Systematic Review Monographic Works. Revista Ciencia y Tecnología El Higo, 13(1), 2–19. https://doi.org/10.5377/elhigo.v13i1.16371